Colposcopy is a critical gynecological examination that helps in the early detection and prevention of cervical cancer. It is a detailed assessment of the cervix, vagina, and external genital area using a special magnifying device called a colposcope.

The examination allows the doctor to identify tissue changes that cannot be seen with the naked eye. If suspicious areas are noticed, a small tissue sample (biopsy) may be taken for further analysis.
When is a colposcopy needed?
Colposcopy is most often performed in the following situations:
• abnormal Pap test result,
• positive finding for high-risk HPV,
• suspicious appearance of the cervix,
• unexplained bleeding or discharge, especially after intercourse or during menopause,
• persistent inflammation or unsatisfactory Pap test results,
• follow-up after treatment of cervical changes,
• conservative monitoring of changes that do not yet require surgery,
• suspicion that changes may extend into the vagina or external genital area.
The goal of the examination is to determine whether a change is present, how serious it is, and what the best next step should be.
Pap test and indications for colposcopy
The Pap test examines cervical cells to detect early changes and prevent cancer. Low-risk findings (such as mild cell changes or unclear cells without high-risk HPV) are unlikely to show serious abnormalities on colposcopy, including severe dysplasia. In such cases, colposcopy is not immediately required, and a repeat Pap test the following year is sufficient.
If abnormal Pap test results persist—exceptionally mild changes combined with a positive high-risk HPV result—colposcopy is recommended.
Some Pap test findings are associated with more serious cervical changes, such as high-grade lesions (HSIL) or atypical cells that cannot exclude high-grade changes (ASC-H). When high-grade changes are suspected, there is also a possibility of an invasive cervical cancer. In such cases, immediate colposcopy is recommended.
Current colposcopy guidelines are based on the estimated risk of high-grade lesions. If the risk is above 25% (based on HPV results, cytology, and clinical history), immediate treatment may sometimes be acceptable. If the risk of CIN3 or more severe changes (CIN3+) is above 4%, colposcopy is indicated.
What to expect during a colposcopy
No special preparation is usually required. The examination may be more difficult during menstruation because blood can obstruct visibility. The doctor prepares all necessary equipment to ensure the procedure is quick and as comfortable as possible.
- Position: The patient lies on an exam table with the legs supported.
- Privacy: A protective sheet covers the lower part of the body.
- Examination: A speculum is inserted, and the cervix and vagina are examined with the colposcope.
- Acetic acid: A 5% acetic acid solution is applied to the cervix, causing abnormal cells to turn white temporarily.
- Lugol’s iodine: Healthy tissue stains brown, while abnormal areas remain pale.
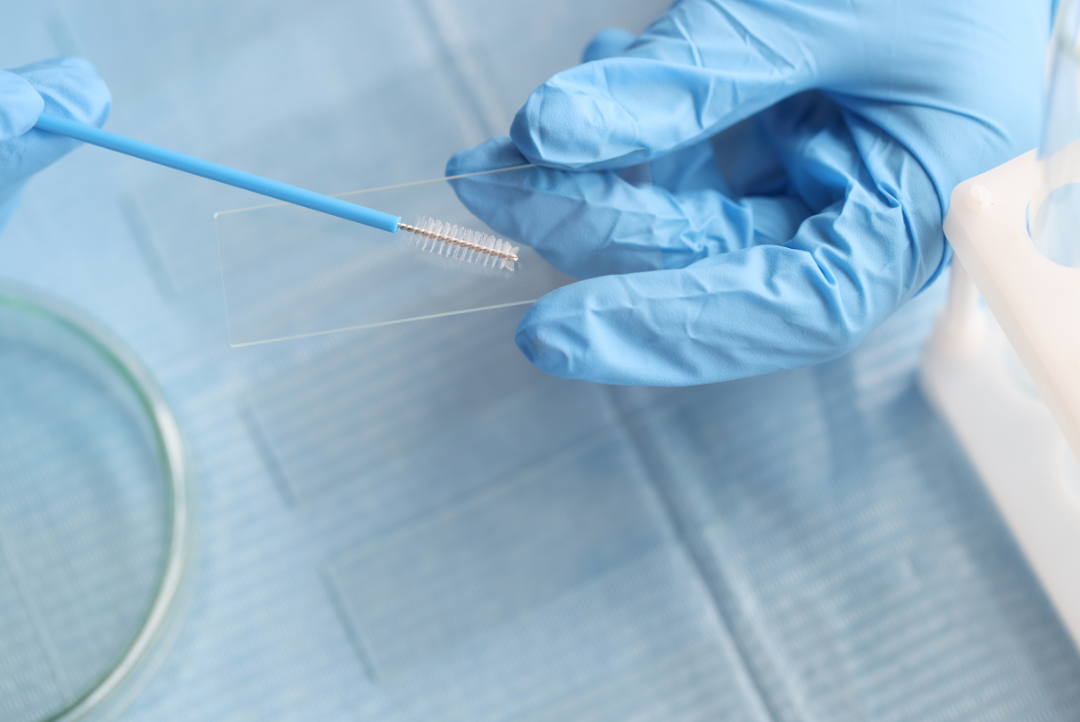
- Biopsy: If necessary, a small tissue sample is taken, and a solution may be applied to stop bleeding.
The examination typically lasts 10–20 minutes.
Expertise and the importance of high-quality colposcopy
Colposcopy requires specialized knowledge and extensive experience to ensure reliable results. Studies show that some significant changes may be missed—between 13% and 69% of high-grade precancerous or invasive lesions can go undetected.

There is also an advanced method—digital colposcopy—which uses a digital camera and LED light. Images appear on a monitor, allowing the doctor, patient, and clinical team to see the findings in real time. Images can also be saved for documentation and follow-up.
What to expect during the examination
Most women feel only mild pressure or warmth, rarely pain. The examination is safe, and the doctor explains each step. Patients may request a pause or ask questions at any time. Good communication and relaxing the pelvic muscles significantly reduce discomfort. Colposcopy is a safe and critical examination for early detection and prevention of cervical cancer. Clear communication, understanding of the process, and trust in the doctor help make the experience more comfortable and reduce anxiety.
The role of regular gynecological exams and Pap testing
Everything begins with regular check-ups with a gynecologist, which are essential for monitoring women’s health. During these appointments, the doctor evaluates the cervix, vagina, and other reproductive organs and provides recommendations for further testing or follow-up.
One of the most essential screenings is the Pap test, which detects early cell changes and helps prevent cervical cancer. Detailed information about the Pap test is available on our blog, including when it should be performed and how to interpret the results.
Regular gynecological exams, Pap testing, and trust in your gynecologist ensure that your reproductive health is well monitored, enabling timely protection and peace of mind.